A night out is rare. Preeclampsia isn’t.


Preeclampsia can happen to any woman, during any pregnancy
Now that you’re pregnant, or considering pregnancy, you know that certain things you once took for granted—like sleep, me time, even clean laundry—will become rare.
But one thing that isn’t rare is preeclampsia.
5–8%
of all pregnancies are affected by preeclampsia1,2

15%
of premature births in the U.S. are caused by preeclampsia3
What is preeclampsia?
Preeclampsia is a serious disease related to high blood pressure that usually occurs in the second half of pregnancy. Preeclampsia affects 5–8%1,2 of all pregnancies and can happen to any woman, during any pregnancy.
What is early onset preeclampsia?
When high blood pressure results in the delivery of a baby before 34 weeks of pregnancy, it’s called “early onset preeclampsia” and is often a more dangerous form of the disease. Left untreated, it can lead to life-threatening complications for both you and your baby.
That’s why it’s important to talk to your doctor about how you can be screened for early onset preeclampsia.
Am I at an increased risk?*
Because preeclampsia can affect any pregnancy, all women should consider screening. However, the following risk factors may increase your chances of developing it.
- First pregnancy
- You or a close family member has had preeclampsia
- Advanced maternal age
- Pregnant with more than one baby (e.g., twins)
- Fertility treatment
- History of obesity, hypertension, diabetes, renal disease, blood disorders or lupus
What are the symptoms?*
Preeclampsia symptoms can disguise themselves as normal pregnancy symptoms, so being aware of them is key. Some symptoms include:4
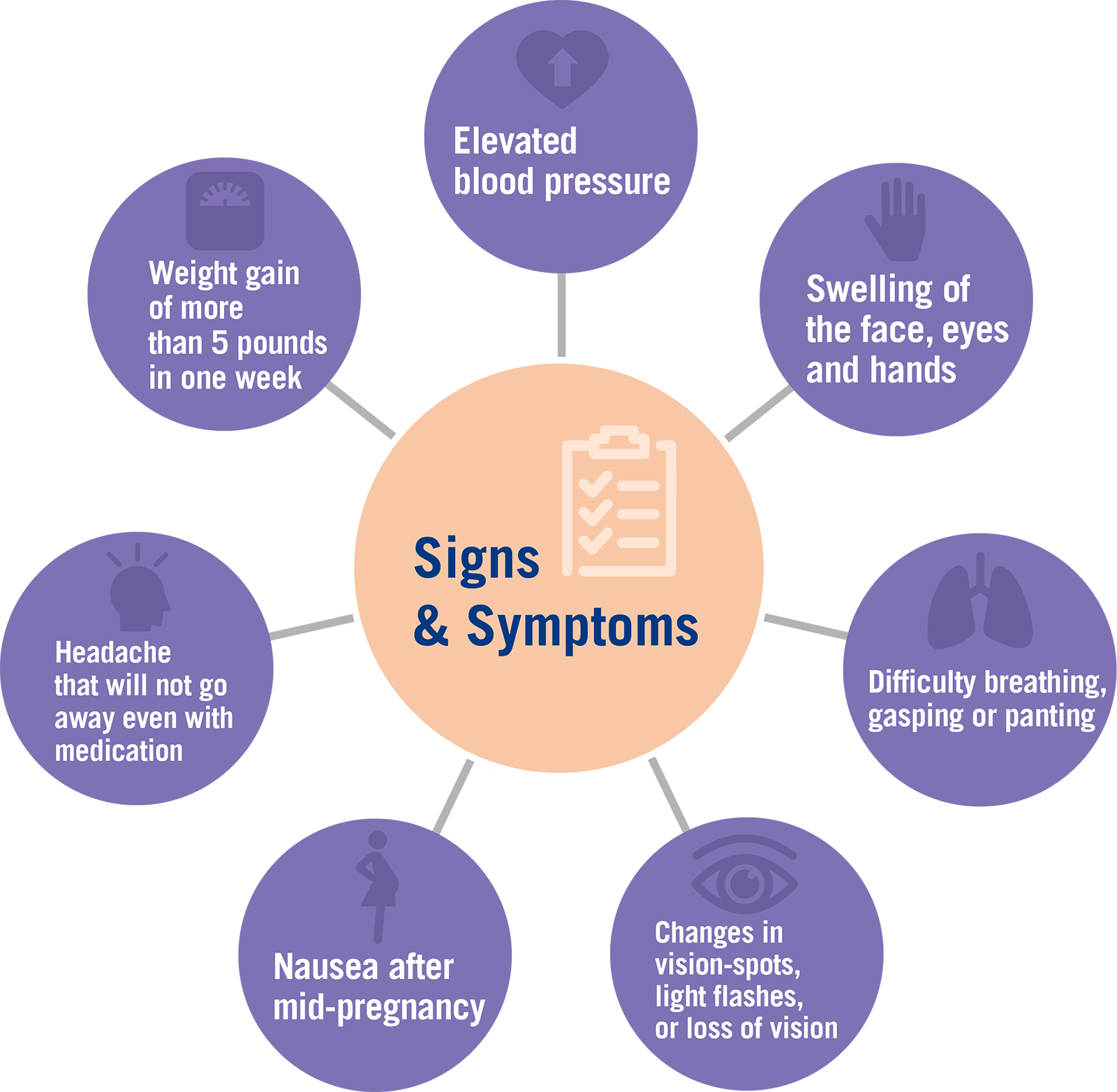
Because of the broad range of symptoms, including no symptoms at all, preeclampsia can often go undiagnosed. That’s why Eurofins NTD has created a screening tool to help you and your doctor more accurately assess your risk.
Get the support you need
Want more information? The Preeclampsia Foundation offers:
- Educational materials and videos
- Research updates
- Testing options
- A community of women and families who’ve been affected by the disease
Earlier insight means more opportunity
PreeclampsiaScreen℠ | T1 is a first-trimester screening test that measures the presence of three biological “markers” in your blood. When detected at certain levels, these markers can indicate a higher risk of developing early onset preeclampsia.
A high-risk test result gives you the chance to take some easy steps to manage your pregnancy.
PreeclampsiaScreen℠ | T1 analyzes three biochemical markers: PAPP-A (pregnancy-associated plasma protein-A), PlGF (placental growth factor) and AFP (alpha fetoprotein). Together, these three biochemical markers, along with a special sonographic and blood pressure measurement, can contribute to accurate prediction of risk for early onset preeclampsia in the first-trimester. Pregnant women can take the test as early as 11 weeks. It has a 91% detection rate and only a 5 percent false positive rate.
The PreeclampsiaScreen℠ | T1 test has been reviewed and approved by the New York State Department of Health. To view the validation paper, please click here.
About Eurofins NTD
For more than 30 years, Eurofins NTD has pioneered the research and development of prenatal screening protocols for Open Neural Tube Defects, Down syndrome, trisomy 18 and trisomy 13. Today, Eurofins NTD serves universities, medical centers, hospitals, laboratories, obstetricians and maternal fetal medicine specialists worldwide—providing risk assessment services that help healthcare professionals and patients make more informed decisions.
*Having one or more of these risk factors or symptoms does not mean you will develop preeclampsia, but it may point to the need for early screening to help further evaluate and refine your risk.
References
- Srinivas SK, Edlow AG, Neff PM, Sammel MD, Andrela CM, Elovitz MA. Rethinking IUGR in preeclampsia: dependent or independent of maternal hypertension? J Perinatol. 2009;29(10):680–4.
- Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestationalhypertension, United States, 1987–2004. Am J Hypertens. 2008;21(5):521–6.
- March of Dimes. Preeclampsia. Available at https://www.marchofdimes.org/complications/preeclampsia.aspx. Accessed March 16, 2018.
- Preeclampsia Foundation. Signs & symptoms. 2016 Mar 29. Available at http://www.preeclampsia.org/signs-and-symptoms. Accessed March 1, 2018.
